Spinal Muscular Atrophy (SMA) Type 1, historically known as Werdnig-Hoffmann Disease, is a severe genetic disorder that affects the motor neurons in the spinal cord. As the most common and most severe form of SMA, it primarily impacts infants, leading to significant muscle weakness and respiratory challenges.
In this guide, we will explore the causes, symptoms, diagnostic processes, and the revolutionary treatments available in 2026.
What is SMA Type 1 (Werdnig-Hoffmann Disease)?
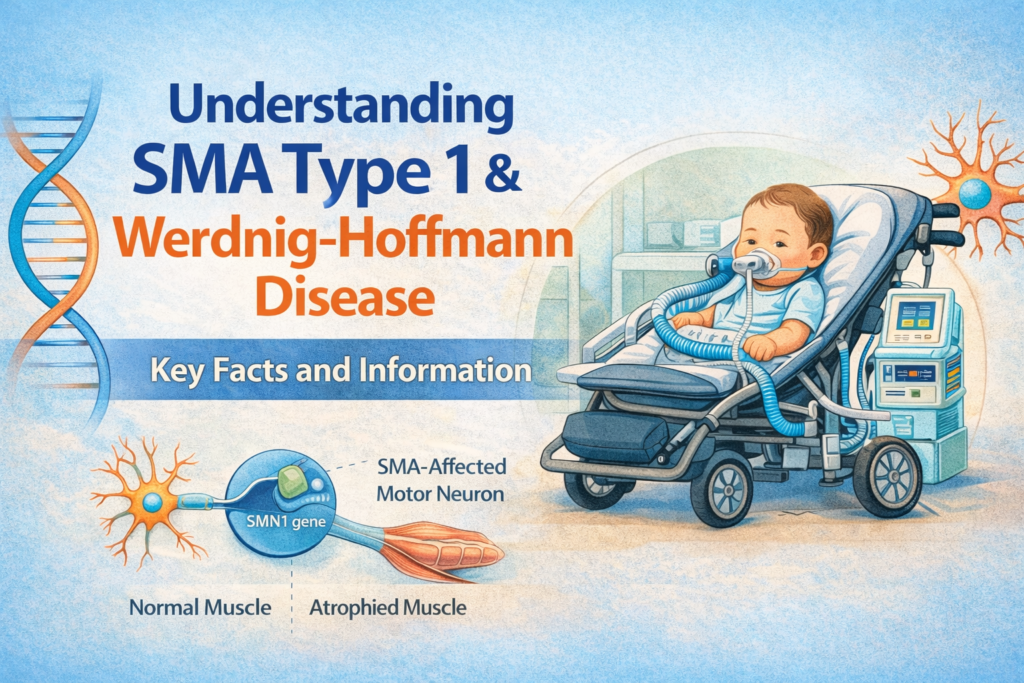
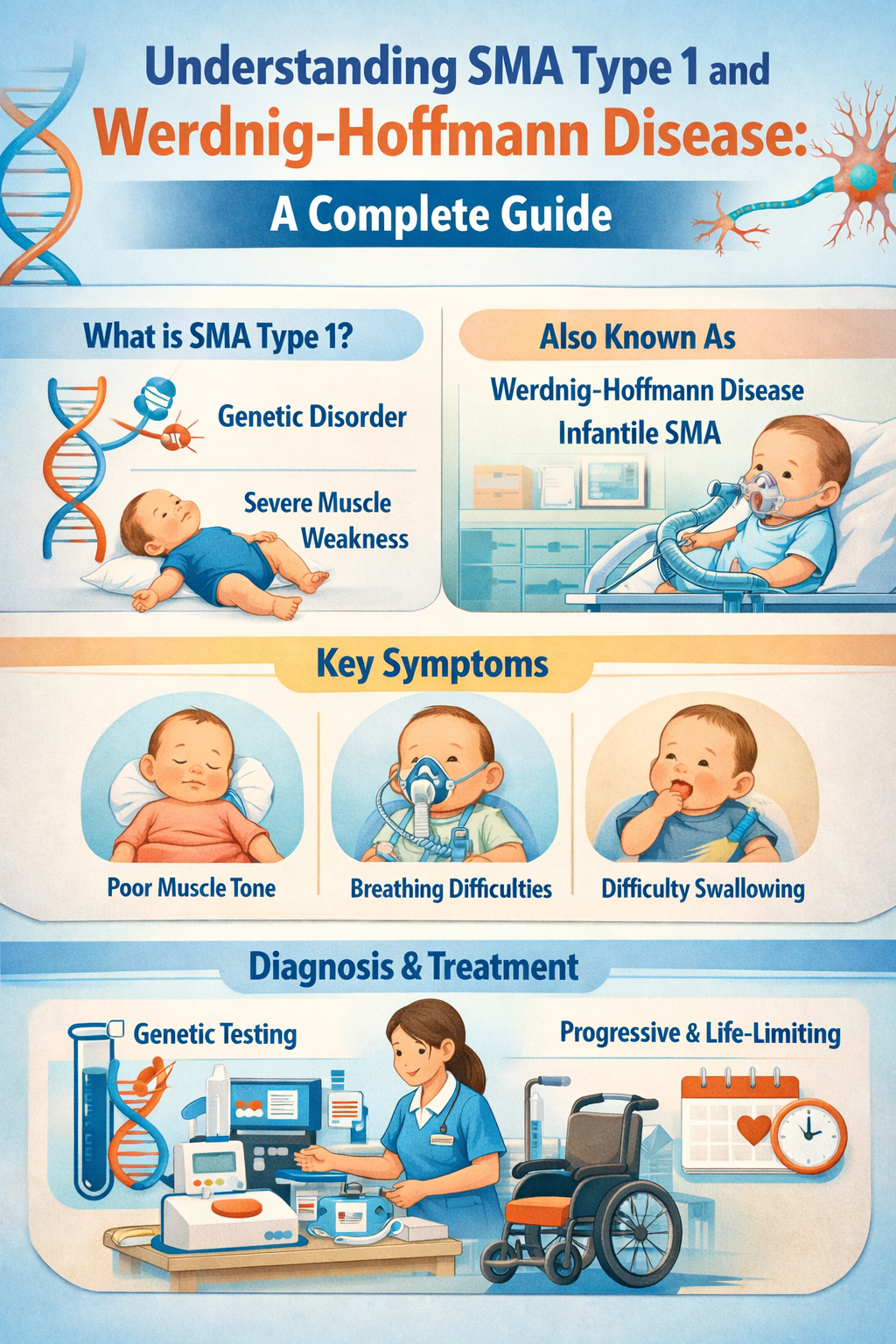
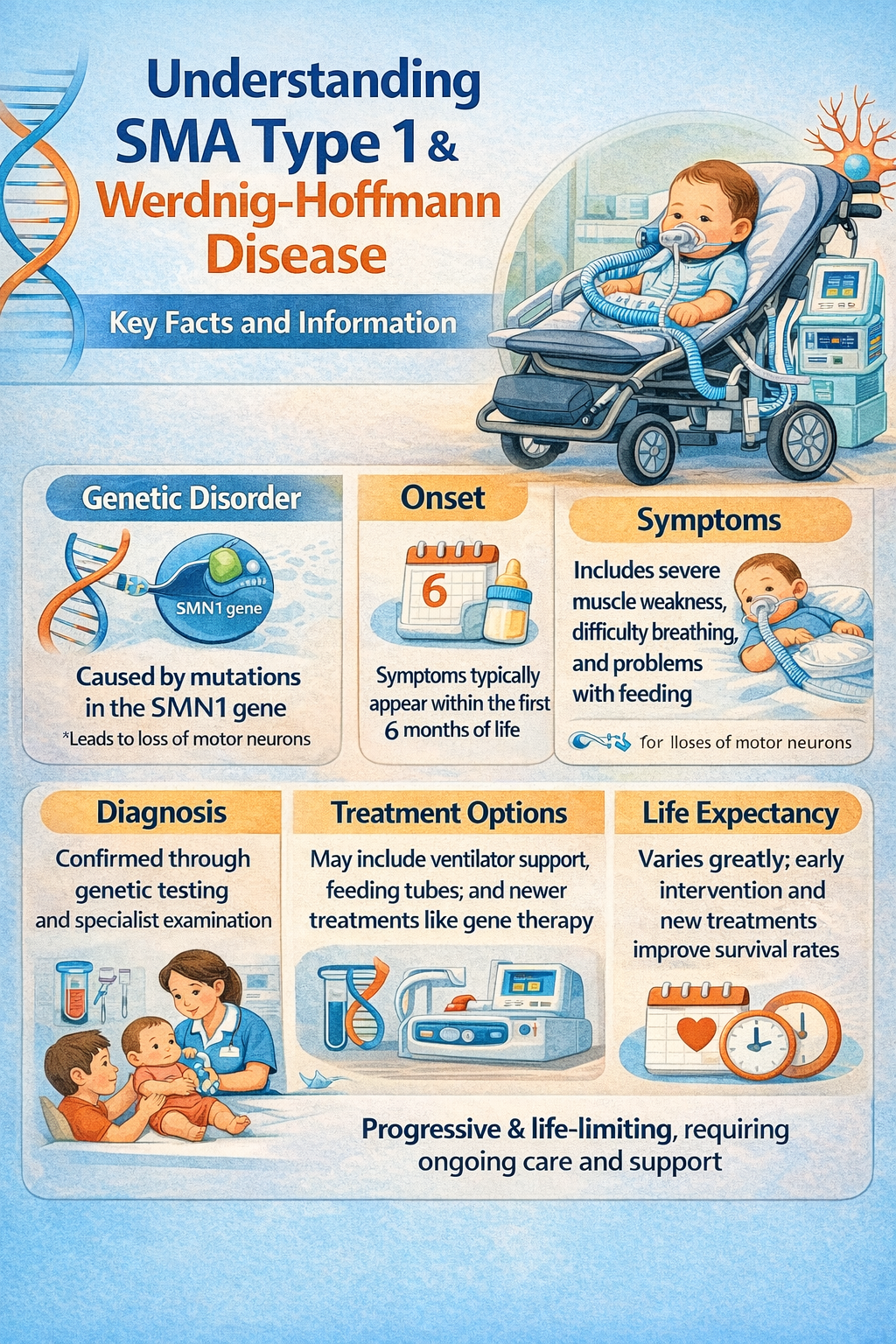
SMA Type 1 is a rare neuromuscular condition characterized by the loss of lower motor neurons. These neurons are responsible for sending signals from the brain to the muscles. When these signals fail, muscles begin to waste away (atrophy).
Named after researchers Guido Werdnig and Johann Hoffmann, who first described the condition in the 1890s, this disease is typically diagnosed within the first six months of an infant’s life. Without intervention, it has historically been the leading genetic cause of infant mortality.
The Genetic Cause: The SMN1 Gene
The root cause of SMA Type 1 is a mutation or deletion in the Survival Motor Neuron 1 (SMN1) gene. This gene is responsible for producing the SMN protein, which is vital for the survival of motor neurons.
Humans also have a “back-up” gene called SMN2. However, SMN2 is less efficient at producing functional proteins. The severity of the disease often depends on how many copies of the SMN2 gene an individual has; infants with SMA Type 1 typically have only two copies of SMN2.
Key Symptoms and Early Signs
Symptoms of Werdnig-Hoffmann Disease often appear suddenly or within weeks of birth. Parents and caregivers should look for:
- Generalized Muscle Weakness: Often referred to as “floppy baby syndrome” (hypotonia).
- Lack of Head Control: The infant cannot hold their head up independently.
- Weak Cry and Difficulty Swallowing: Bulbar muscle weakness can make feeding dangerous, leading to aspiration risks.
- Bell-Shaped Torso: Due to weak abdominal muscles and the use of the diaphragm for breathing.
- Lack of Milestone Achievement: The child will never be able to sit up unassisted, crawl, or walk.
- Tongue Fasciculations: Small, involuntary tremors or flickering of the tongue.
Modern Diagnostic Procedures
Early diagnosis is critical. If a pediatrician suspects SMA, they will utilize the following methods:
- Genetic Testing: This is the gold standard. A simple blood test can identify the deletion of the SMN1 gene.
- Newborn Screening: By 2026, many countries have integrated SMA testing into standard newborn screening panels, allowing for treatment before symptoms even begin.
- Electromyography (EMG): Used occasionally to measure the electrical activity of muscles, though genetic testing has largely replaced this for SMA.

Treatment Options in 2026: A New Era of Hope
Until recently, treatment for SMA Type 1 was purely palliative. Today, three FDA-approved therapies have transformed the prognosis for these children:
1. Gene Replacement Therapy (Zolgensma)
Zolgensma is a one-time intravenous infusion that delivers a functional copy of the SMN1 gene directly into the patient’s cells. It is most effective when administered early, ideally before the onset of symptoms. You can find more information on the official Zolgensma website.
2. RNA-Based Therapy (Spinraza)
Nusinersen (Spinraza) was the first approved treatment for SMA. It is an antisense oligonucleotide (ASO) injected into the spinal fluid (intrathecal) that helps the SMN2 gene produce more functional protein. Learn more at the Spinraza Patient Portal.
3. Oral Medication (Evrysdi)
Risdiplam (Evrysdi) is a daily liquid medication taken by mouth or feeding tube. Like Spinraza, it targets the SMN2 gene to increase protein production. Details are available via the Evrysdi Resource Center.
Supportive Care and Management
While medical therapies treat the genetic cause, multidisciplinary care is essential for quality of life:
- Respiratory Support: Many infants require Non-Invasive Ventilation (NIV) like BiPAP to assist with breathing, especially during sleep.
- Nutritional Support: Because of swallowing difficulties (dysphagia), many children require a G-tube (gastrostomy tube) to ensure adequate caloric intake.
- Physical Therapy: Specialized exercises help maintain joint flexibility and prevent contractures.
- Occupational Therapy: Provides adaptive equipment to help children interact with their environment.
The Importance of Early Intervention
The “Time is Tissue” rule applies strictly to SMA. Motor neurons, once lost, do not regenerate. This is why 2026 healthcare standards emphasize Pre-symptomatic Treatment. If a child is treated within the first days of life through newborn screening results, they may achieve developmental milestones—like sitting and walking—that were previously thought impossible for Type 1 patients.
Final Thoughts
SMA Type 1 (Werdnig-Hoffmann Disease) is no longer the “death sentence” it was a decade ago. With the advent of gene therapy and specialized care, children are living longer, stronger lives.
If you are a parent or caregiver, resources like Cure SMA provide invaluable community support and the latest research updates. Always consult with a pediatric neurologist to discuss the best path forward for your child